February 6, 2019
Researchers at the Weizmann Institute of Science have identified a genetic ‘switch’ that is only active when nerves are injured – recently reported in Molecular Cell.
Genes that encode proteins are usually active in so many tissues and in so many different situations that manipulating them for therapeutic purposes can be tricky. Blocking or enhancing their activity may help cure disease in one organ while causing unwanted side effects in others. But there are genes that don’t encode proteins. Among them are those that encode long regulatory molecules called lncRNAs, and these are dedicated specialists:
They tend to be expressed only in specific tissues and under specific circumstances. The researchers found a lncRNA gene plays a crucial role in nerve repair and might help develop precisely targeted therapies.
Because the lncRNAs – long non-coding RNAs, pronounced link-RNAs – don’t provide recipes for making proteins, they had been ignored for years. Only in the past decade or so have they started revealing themselves as important regulators of the genome; they are involved, for example, in controlling cell growth and division both during fetal development as well as in the adult organism.
“The human genome has more than 20,000 lncRNA genes – probably more than genes coding for proteins – and so far we know the function of only a tiny fraction of them,” said team leader Dr Igor Ulitsky of the Biological Regulation Department.
Do lncRNAs play a role?
The greatest diversity of lncRNA genes expression is found in the neural tissues (along with the testes), so Ulitsky’s team – Dr Rotem Ben-Tov Perry, Hadas Hezroni and Micah Goldrich – set out to explore the function of lncRNAs in these tissues in the mammalian body.
In particular, the researchers sought to determine whether lncRNAs play a role in nerve regeneration. After nerve injury, neurons in the legs, arms and rest of the peripheral nervous system can regenerate, regrowing their extensions to repair the damage, but neurons in the central nervous system, that is, the brain and spinal cord, do not have this ability. Why neurons behave so differently in the two systems is not entirely clear, particularly since in both places they have similar “on” and “off” switches for growth. Ulitsky and his colleagues wanted to see whether lncRNAs might help resolve the riddle.
The scientists performed an extensive genetic analysis of mice with injuries to the sciatic nerve. They found that about a week after the injury, when the nerve was regrowing vigorously, expression of a particular lncRNA gene soared tenfold.
They then discovered that this gene – they called it Silc1 – activates a unique regeneration program that repairs damage to the sciatic nerve: It serves as a switch for an adjacent gene known to be involved in regeneration – a switch that is flipped on only in the case of neural regrowth, but not in other types of injury.
A dedicated specialist
Next, the researchers conducted a series of experiments confirming the pivotal role Silc1 plays in nerve regeneration. When they enhanced the expression of Silc1 in neurons in a laboratory dish, the growth of extensions from these cells increased by 40 percent compared with that from unmanipulated neurons.
Conversely, when they blocked the expression of Silc1 in mice by genetic manipulation, the sciatic nerves of the mice regenerated less effectively after injury and their recovery was slower than in mice with an active copy of Silc1. Silc1’s importance to the body is highlighted by the fact that it is one of only about a thousand lncRNA genes that have been conserved in evolution, and by its presence in all mammals, including mice, rats and humans.
Additional experiments showed that Silc1 is a dedicated specialist par excellence: It is expressed only in adults, only after injury to peripheral nerves, and only in nerves coated by the insulating myelin sheath, but not in nerves lacking this wrapping. That is, it is not expressed in the central nervous system.
The ‘specialist’ status of Silc1 suggests that it may help in developing targeted nerve repair therapies that won’t cause unwanted side effects in other tissues.
“Nerve regeneration in the peripheral nervous system is far from perfect, and it’s slow, for example, recovery of function in the sciatic nerve – the longest and widest nerve in the human body that runs about a meter long – can take up to a year,” said Ulitsky.
“In the future, it might be possible to develop therapies that will stimulate this regeneration by manipulating such lncRNAs as Silc1.”
Silc1 may also open a new direction for studies aimed at inducing nerve regeneration in the central nervous system. These studies would need to check whether triggering or stimulating Silc1 expression in nerves lacking the myelin sheath can help damaged nerves regrow. If further studies show this is the case, it might help, for example, in restoring function after injury to the spinal cord.
(l-r) Dr Rotem Ben Tov Perry, Micah Goldrich and Dr Igor Ulitsky
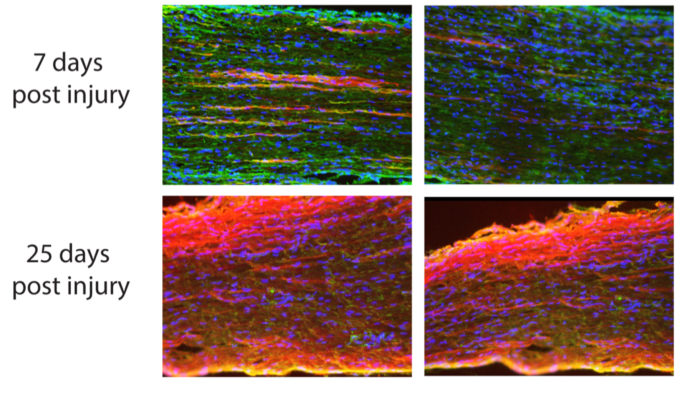
Regeneration of neuronal branches, surrounded by glia cells (whose nuclei are marked by blue dots), in a mouse sciatic nerve, seven days (top) and 25 days (bottom) after injury, viewed with fluorescence microscopy. In mice lacking Silc1 (left column), regeneration is less vigorous – newly regrown branches of neurons (red) are shorter – compared with mice with a functioning copy of Silc1 (right column)