September 16, 2019
New Weizmann Institute of Science research shows heterogeneity in melanoma tumours prevents effective immune responses.
Diversity – at least among cancer cells – is not a good thing. Weizmann research shows that in melanoma, tumours with cells that have differentiated into more diverse subtypes are less likely to be affected by the immune system, thus reducing the chance that immunotherapy will be effective.
The findings of this research, recently published in Cell, may provide better tools for designing personalized protocols for cancer patients, as well as pointing toward new avenues of research into anti-cancer vaccines.
Professor Yardena Samuels of the Institute’s Molecular Cell Biology Department wanted to know why, despite the fact that cancer deaths from melanoma have dropped in recent years thanks to new immunotherapy treatments, many patients do not respond to the therapy.
The reasons for this have not been clear, though the leading hypothesis, supported by a few studies, has been that tumours with more mutations – a higher ‘tumour mutational burden’ – are more likely to respond to immunotherapy. Some patients even spend large sums to undergo radiation or chemical treatments to increase tumour mutations, but a causal relationship between the two has not yet been proven.
Samuels and her colleagues were intrigued by studies that had suggested a different possible correlation – that between heterogeneity (that is, the genetic diversity among tumour cells) and the response to therapy. To investigate this theory, however, the team had to develop a new experimental system to check exactly which factors play a role.
In the study, which was led by Drs Yochai Wolf and Osnat Bartok in Samuels’ lab, the researchers took mouse melanoma cells and exposed them to a type of UV light known to promote this cancer. This increased both the mutations and the cell heterogeneity in the growth. When they injected mice with either these cells or the regular melanoma cells, the irradiated ones multiplied faster and were more aggressive. Despite the fact that these cells had a higher mutational burden – and thus should have been more responsive to immunotherapy – they actually were less likely to be eradicated than those from the original tumour. In other words, although there was a high mutational burden, there was also high heterogeneity, and the researchers hypothesized that the latter was driving the resistance.
Since mutational burden and heterogeneity generally go hand in hand, the researchers needed to find a way to study one without the other. They removed single cells from a culture of an aggressive cancer growth and then grew new cultures from each cell. Thus, they ended up with 22 new cultures, each with a low level of heterogeneity but carrying some random number of mutations.
When they injected these cells into mice, the researchers were surprised to find that all the tumours grew slowly, and even disappeared without immunotherapy – in those with higher and lower mutational burdens alike. To see if the mice’s immune systems were responsible for killing the cancer cells, they repeated the experiment in mice with weakened immune systems. In these the cancer spread rapidly.
To further understand the immune response, the researchers tried the experiment again, this time on mice specifically engineered to lack T cells – the immune cells that are known to fight cancer.
“The results were similar to those in mice with weakened immune systems,” said Wolf.
“When we look at T cells from different tumours, we found much more activity in the homogenous growths, and less in the heterogeneous ones.”
In fact, the researchers found that in the homogeneous growths, T cells had penetrated to the centre of the tumour, while in the heterogeneous ones, they remained on the outside, and there were more T cells of a different type – ones that suppress immune activity.
“We showed the difference between two extremes – highly homogeneous and highly heterogeneous, but most cancers fall somewhere in between,” said Bartok.
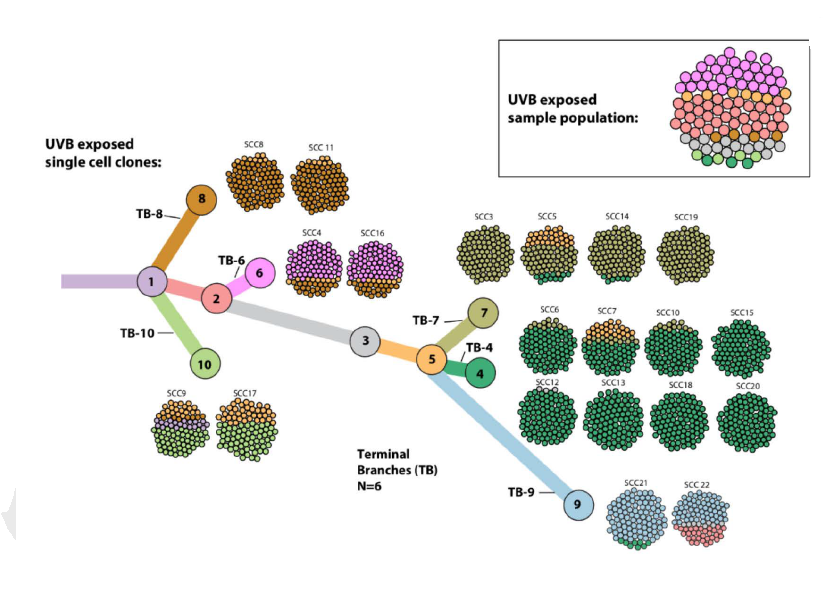
“To systematically generate tumours with intermediate levels of genetic heterogeneity, we created a phylogenetic tree of the parental heterogeneous line, and mapped out how subtypes appear over time. Then we created ‘cocktails’ of homogeneous cell lines based on this tree, with more or less heterogeneous combinations of cells, and injected them into mice.”
As predicted, the more homogeneous the cell cocktail, the easier it was for the mice’s immune systems to eradicate the cancer, whereas the more heterogeneous the tumours were, the more aggressive they became.
“We found that testing the number of cell subtypes and their place on the phylogenetic tree are a much better predictor than mutational burden of the success of immunotherapy,” said Samuels.
“We also went over data from melanoma patients who had undergone immunotherapy, and found a high correlation between these factors and the success of the treatment. Ultimately, we intend to use the experimental system we created to work on developing applicable personalized protocols for cancer patients.”
Also participating in this research were Professor Eytan Ruppin of the National Cancer Institute of the National Institutes of Health (NIH) of the US, Professor Prrro Lea Eisenbach of the Institute’s Immunology Department, Dr Yishai Levin of the Nancy and Stephen Grand Israel National Center for Personalized Medicine at the Institute, Professor Martin Miller of the University of Cambridge, Professor Eli Pikarsky of Hebrew University-Hadassah Medical School, Prof Arie Admon of the Technion –Israel Institute of Technology and Professor Charles Swanton of University College London.
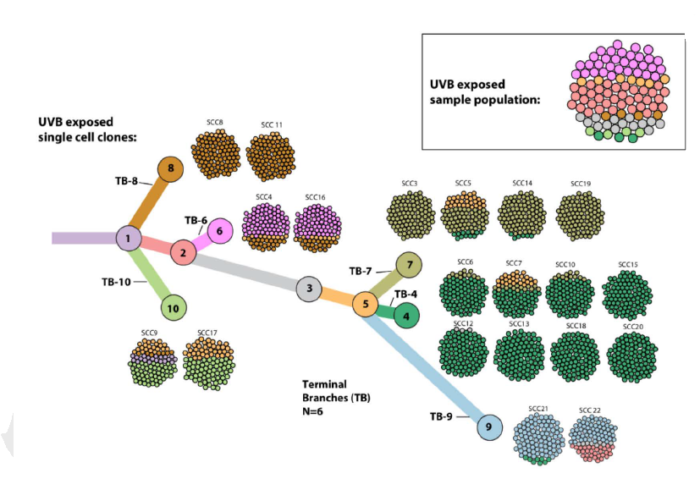
Tumour cells were mapped to a phylogenetic tree according to heterogeneity, enabling the researchers to conduct further experiments
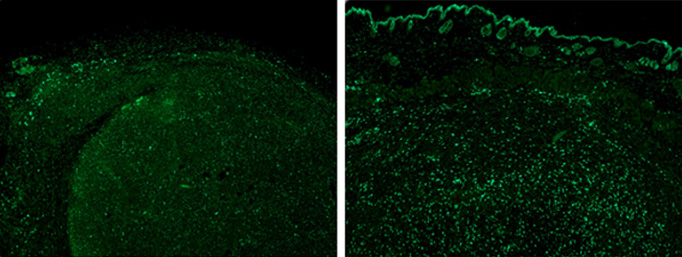
Cancer-killing T cells (green) in heterogeneous (l) and homogeneous (r) melanoma tumours. In the heterogeneous tissue, the T cells remained outside the tumour, while in the the homogeneous tissue they penetrated to the core