September 9, 2020
Pre-clinical studies at the Weizmann Institute of Research suggest a protein called Agrin could limit scarring and promote natural repair mechanisms after a heart attack.
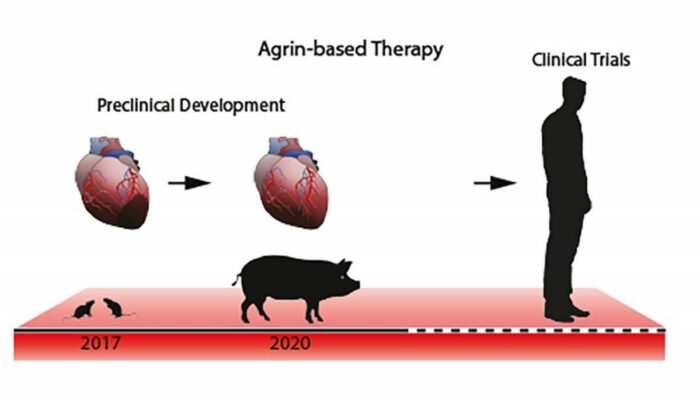
Heart disease is the number one cause of death in the world, surpassing all cancers combined. One of the major difficulties in coming up with new therapies lies in translating basic research findings, typically obtained with mice, into a treatment that works in humans. This gap can be filled by experimenting on pigs, whose hearts beat at a rhythm similar to that of humans and otherwise provide a faithful model – both size-wise and physiologically – of human cardiovascular function.
The Weizmann researchers, in close collaboration with a team from the Technical University of Munich, have now showed that the protein Agrin, previously found to renew damaged heart tissue in mice, promotes heart repair in pigs.
The researchers have also clarified Agrin’s mechanisms of action, which turned out to be similar in mice and pigs, indicating that it’s likely to work similarly in all mammals, including humans. These findings suggest that Agrin might serve as an effective therapy after heart attacks, promoting heart repair and helping to prevent chronic heart failure.
Agrin is naturally present in the supporting heart cells in mouse and human foetuses, and in the hearts of newborn mice – that is, in settings where regeneration is possible – suggesting that it can play a role in heart muscle regeneration. In previous research, a team headed by Professor Eldad Tzahor of Weizmann’s Molecular Cell Biology Department discovered that Agrin “unlocked” a renewal process in injured mouse hearts.
To test whether this protein is likely to help heal human hearts, Tzahor established a collaboration with Professor Christian Kupatt of the Technical University of Munich to study Agrin’s efficacy in pigs.
Senior intern Dr Kfir Baruch Umansky led the study, in which the researchers administered a synthetic form of human Agrin protein to the hearts of pigs that had been exposed to an injury simulating a heart attack. Working with Kupatt’s team in a hospital setting – and using clinical protocols and tools relevant to treating human patients – Umansky and colleagues found that a single dose of Agrin reduced scarring and improved heart function after the injury.
The heart’s pumping capacity, measured by the volume of blood ejected with every beat, was significantly enhanced. In addition, the Agrin treatment prevented the rise of pressure in the heart’s main pumping chamber, which grows after a heart attack because the scarred heart becomes stiff and less effective at pumping. Since this parameter is a predictor of the subsequent risk of heart failure, the researchers suggest that Agrin can serve as a preventive therapy against this major complication of heart attacks.
Focusing in greater detail on Agrin’s mechanism of action, the researchers found in both pig and mouse models that Agrin induces a broad range of repair processes, which is probably why a single dose of the protein produced potent effects lasting up to one month after the treatment. The protein triggered a mild proliferation of heart muscle cells, which normally don’t divide, and, perhaps more importantly, protected them from dying, particularly in the border zone around the injury site, thus preventing the spread of scar tissue.
In addition, Agrin beneficially altered the immune response to the injury within the heart muscle: It curbed inflammation by reducing the activation of immune cells called macrophages that are responsible for the early release of inflammatory substances. Not only that, the scientists found that Agrin protected existing blood vessels within the heart muscle and stimulated the growth of new ones.
In the course of the study, the method that worked best for delivering Agrin to the injured pig heart was to inject it into the coronary artery using the same type of catheter that is generally used in angioplasty to widen obstructed arteries. This suggests that patients undergoing angioplasty could have a dose of Agrin administered at the same time.
Agrin’s effectiveness in such large animals as pigs, together with the ease of delivery, could pave the way to its use in human patients. Scarring and loss of heart function are prevalent after a heart attack, and the study’s findings suggest we may finally have a way to limit and possibly even reverse the damage, improving the outcome of heart attacks and perhaps averting their complications.
“The road from basic research to the clinic is long and often bumpy, so our study in pigs provides a critical step in this direction,” Tzahor said.
This study was made possible, in part, by a new program that aims to bridge the gap between promising basic science breakthroughs at the Institute and commercial application. Called IDEA (Innovation, Development, Enhancement and Acceleration), it is an initiative of Yeda, Weizmann’s technology transfer arm.
Study participants included Dr Elad Bassat, Dr David Kain and Renee Cohen-Rabi from Weizmann’s Molecular Cell Biology Department; Dr Andrea Baehr, Victoria Jurisch, Dr Katharina Klett, Dr Tarik Bozoglu, Dr Nadja Hornaschewitz, Professor Karl Ludwig Laugwitz and Dr Rabea Hinkel from the Technical University of Munich; Dr Olga Solyanik, Dr Bartolo Ferrero, Dr Clemens Cyran and ProfessorOliver Soehnlein from the Ludwig Maximilian University of Munich; and Dr Markus Krane from the German Heart Centre Munich.
Professor Eldad Tzahor is Head of the Yad Abraham Research Center for Cancer Diagnostics and Therapy; his research is also supported by the Zuckerman STEM Leadership Program; the Dr Dvora and Haim Teitelbaum Endowment Fund; and Pearl C. Vapnek.
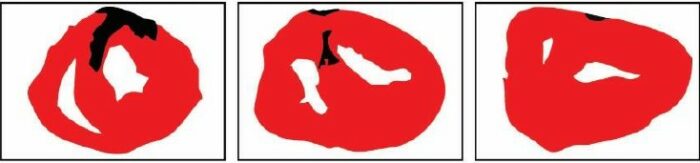
Computerised images of pig hearts after a heart attack. The volume of scar tissue (black) is significantly larger in untreated pigs (left) compared with pigs treated with a single (centre) or double (right) dose of Agrin
Professor Eldad Tzahor